The age at which a woman undergoes menopause significantly influences her risk of developing dementia later in life. Specifically, **earlier menopause (before age 50)** is linked to a higher risk of cognitive decline and dementia, including Alzheimer’s disease, while **later menopause (after age 52)** tends to be associated with better cognitive outcomes and lower dementia risk[1][5][7].
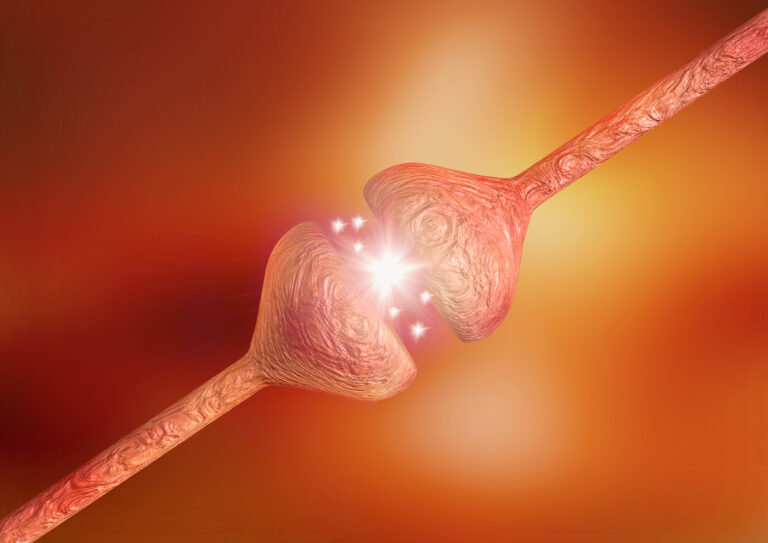
Menopause marks the end of a woman’s reproductive years and is characterized by a sharp decline in estrogen levels. Estrogen plays a crucial role in brain health by supporting neuronal communication, regulating inflammation, and protecting brain structures such as the hippocampus, which is vital for memory and cognition. When menopause occurs earlier, the brain is exposed to lower estrogen levels for a longer period, which may accelerate neurodegenerative processes and increase dementia risk[1][5].
Research from the Framingham Heart Study Offspring cohort found that women who experienced menopause at or before age 49 had **lower hippocampal volume**, a brain region critical for memory, compared to those who underwent menopause at ages 50-51. This reduction in hippocampal volume is a known marker of increased dementia risk[1]. Additionally, earlier menopause correlates with poorer performance across multiple cognitive domains, including abstract reasoning and visuospatial skills[1][7].
Hormone replacement therapy (HRT), which supplements estrogen (sometimes combined with progesterone), has been studied extensively for its potential to mitigate dementia risk associated with menopause. The timing of HRT initiation is critical:
– **Starting HRT within five years of menopause onset** is associated with a **20% to 32% reduction in Alzheimer’s disease risk**. This early initiation appears to provide neuroprotective effects by compensating for the sudden estrogen loss and supporting brain function during a vulnerable period[2][3][4].
– Conversely, **beginning HRT after age 65 or more than 10 years post-menopause** may **increase dementia risk by up to 38%**, especially when combined estrogen-progestin therapies are used. Late initiation may fail to confer benefits and could even exacerbate cognitive decline, possibly due to changes in brain receptivity to hormones or other age-related factors[2][3][4][6].
The biological rationale behind this timing effect is that estrogen receptors in the brain may become less responsive or fewer in number as women age, reducing the effectiveness of hormone therapy started late. Early HRT may help maintain neuronal health and reduce Alzheimer’s pathology, while late HRT might not reverse established neurodegeneration and could have adverse effects[3][4].
Other reproductive factors also influence dementia risk. For example, a longer reproductive lifespan (the time between menarche and menopause) and higher lifetime estrogen exposure are generally linked to better cognitive outcomes. Women with more live births and higher serum estradiol levels tend to perform better on cognitive tests, suggesting that cumulative estrogen exposure throughout life supports brain health[1].
In summary, **earlier menopause is a risk factor for dementia**, likely due to prolonged estrogen deficiency affecting brain structure and function. Hormone replacement therapy can modify this risk, but its benefits depend heavily on starting treatment soon after menopause rather than later in life. These findings underscore the importance of considering reproductive history and hormone therapy timing in strategies aimed at reducing dementia risk in women.
—
**Sources:**
[1] PubMed: Association between reproductive factors and neurocognitive markers, 2023
[2] Being Patient: Menopause, Hormone Therapy, and Alzheimer’s Prevention, 2025
[3] Psychiatric Times: Alzheimer Disease Risk and Hormone Replacement Therapy Timing, 2025
[4] Drugs.com: Age at Start of Estrogen Therapy and Alzheimer Disease Risk, 2025
[5] Neurology Journal: Menopause Age and Estradiol-Based Cognitive Outcomes, 2022
[6] EM