Aging increases susceptibility to sepsis through multiple interconnected biological and physiological changes that weaken the body’s ability to detect, respond to, and recover from infections. As people grow older, their immune system undergoes a gradual decline known as immunosenescence, which impairs both innate and adaptive immune responses. This diminished immune function means that older adults are less capable of mounting effective defenses against invading pathogens, making infections more likely to progress to severe systemic inflammation and sepsis.
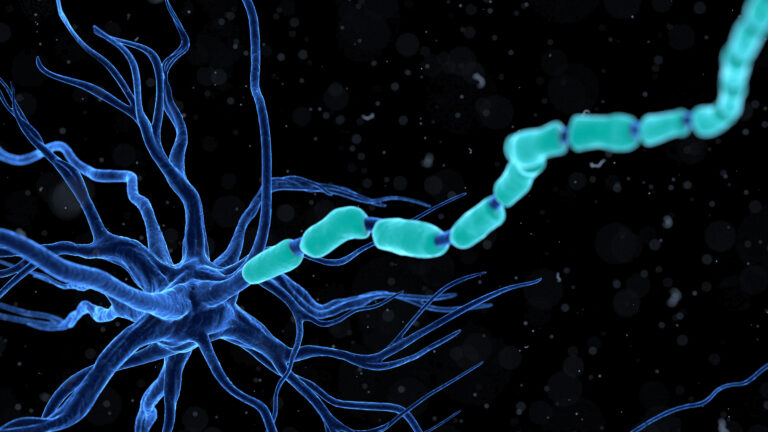
One key factor is the decline in immune cell function. With age, the production and activity of critical immune cells such as neutrophils, macrophages, and lymphocytes decrease. Neutrophils, which are frontline defenders against bacterial infections, show reduced chemotaxis (movement toward infection sites), impaired phagocytosis (engulfing pathogens), and diminished ability to kill microbes. Similarly, macrophages become less efficient at clearing pathogens and dead cells, and T and B lymphocytes exhibit reduced proliferation and antibody production. This overall immune weakening delays infection control and allows pathogens to spread more easily, increasing the risk of sepsis.
In addition to immune cell dysfunction, aging is associated with chronic low-grade inflammation, often called “inflammaging.” This persistent inflammatory state can dysregulate immune responses, making them less precise and more damaging. When an infection occurs, the aged immune system may overreact or fail to resolve inflammation properly, contributing to the exaggerated systemic inflammatory response characteristic of sepsis.
Mitochondrial dysfunction also plays a crucial role in the increased vulnerability of older adults to sepsis. Mitochondria, the energy-producing organelles in cells, become less efficient with age, leading to decreased cellular energy production and increased generation of reactive oxygen species (ROS). During sepsis, this mitochondrial impairment worsens, especially in vital organs like the heart, contributing to organ dysfunction and failure. The aged heart, for example, shows a greater decline in mitochondrial respiratory capacity when exposed to inflammatory stimuli, which exacerbates cardiac dysfunction during sepsis.
Furthermore, aging often comes with multiple chronic health conditions such as diabetes, lung disease, and kidney impairment. These comorbidities further compromise the immune system and organ function, increasing the likelihood that infections will escalate to sepsis. Hospitalization and surgical procedures, more common in older adults, also raise the risk of acquiring infections that can lead to sepsis.
The skin and mucosal barriers, which serve as the first line of defense against pathogens, become thinner and less effective with age. This makes older individuals more prone to skin infections and breaches that can serve as entry points for bacteria. Gastrointestinal infections are also more frequent and severe in the elderly, partly due to changes in gut microbiota and reduced mucosal immunity, further increasing sepsis risk.
Cognitive decline and frailty in the elderly can delay recognition of infection symptoms, leading to late diagnosis and treatment of sepsis. Symptoms like confusion or disorientation may be mistaken for other age-related conditions, allowing the infection to progress unchecked.
In summary, aging increases susceptibility to sepsis through a combination of immune system decline, chronic inflammation, mitochondrial dysfunction, weakened physical barriers, presence of chronic diseases, and delayed symptom recognition. These factors create a perfect storm that makes infections more severe and sepsis more likely and deadly in older adults.