Alzheimer’s disease is a progressive and irreversible neurological disorder that affects millions of people worldwide. It is the most common cause of dementia, a condition that causes a decline in cognitive function, including memory loss, confusion, and difficulty with daily tasks. While the physical symptoms of Alzheimer’s disease are well-known, such as the loss of memory and ability to communicate, the emotional impact of this disease is often overlooked.
Emotional processing is an essential aspect of our well-being and involves our ability to identify, understand, and regulate our emotions. This process is essential for our relationships, decision-making, and overall mental health. However, in the case of Alzheimer’s disease, the brain’s degeneration affects the emotional processing abilities of individuals.
How Emotional Processing Works
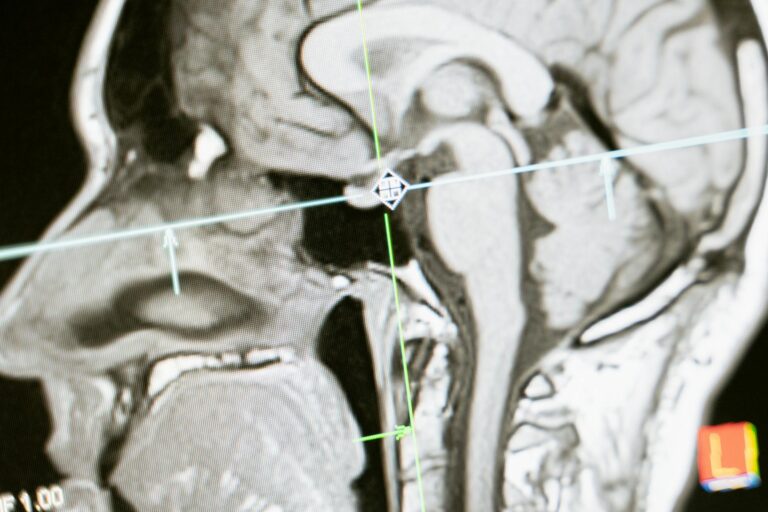
Emotional processing involves several regions of the brain, including the amygdala, hippocampus, and prefrontal cortex. The amygdala is responsible for identifying emotions and triggering emotional responses. The hippocampus helps us remember and store emotional memories. The prefrontal cortex regulates our emotions and helps us make rational decisions based on them.
When we experience an emotion, such as happiness or anger, the amygdala sends signals to the hippocampus to store that emotional memory. The prefrontal cortex then helps us regulate that emotion and respond appropriately. This process happens seamlessly for most people, but it becomes disrupted in individuals with Alzheimer’s disease.
Emotional Processing in Alzheimer’s Disease
As Alzheimer’s disease progresses, it damages the regions of the brain responsible for emotional processing. This damage can cause individuals to have difficulty identifying, understanding, and regulating their emotions. They may also struggle to empathize with others or express their own emotions.
One of the earliest signs of Alzheimer’s disease is changes in mood and behavior. Individuals may become irritable, anxious, or withdrawn. They may also have difficulty controlling their emotions and may have sudden outbursts or mood swings. These changes can be confusing and distressing for both the individual and their loved ones.
As the disease progresses, individuals may also lose the ability to recognize and respond to familiar emotions in others. They may become apathetic or show little interest in activities that used to bring them joy. This can lead to social isolation and feelings of loneliness.
The Impact of Emotional Processing on Caregivers
Emotional processing is not only affected in individuals with Alzheimer’s disease, but it can also have a significant impact on their caregivers. As caregivers witness their loved ones’ decline and struggle to cope with their changing emotions and behaviors, it can take a toll on their mental health.
Caregivers may experience feelings of guilt, frustration, and sadness as they watch their loved one’s personality change. They may also feel overwhelmed and stressed as they try to manage their loved one’s care needs and emotions. Research has shown that caregivers of individuals with Alzheimer’s disease have higher rates of depression, anxiety, and other mental health issues.
Coping with Emotional Changes in Alzheimer’s Disease
While Alzheimer’s disease can impact emotional processing, there are ways for individuals and caregivers to cope with these changes.
– Seek support: It is crucial for individuals with Alzheimer’s disease and their caregivers to seek support from others. This can include joining a support group, talking to a therapist, or simply having a close friend or family member to confide in.
– Practice self-care: Caregivers must take care of their own physical and emotional well-being. This can include getting enough rest, eating well, and engaging in activities that bring joy and relaxation.
– Use non-verbal communication: As verbal communication becomes more challenging for individuals with Alzheimer’s disease, non-verbal cues such as facial expressions, gestures, and touch become important forms of communication.
– Focus on the present: Instead of dwelling on the past or worrying about the future, focus on the present moment. Individuals with Alzheimer’s disease may struggle to remember recent events, but they can still enjoy present experiences.
– Stay calm and patient: When caring for someone with Alzheimer’s disease, it is important to remain calm and patient. Using a gentle tone and approach can help alleviate potential frustration or agitation in the individual.
Conclusion
Emotional processing plays a crucial role in our overall well-being, and its disruption in Alzheimer’s disease can have a profound impact on individuals and their caregivers. While this disease can be challenging to manage, there are ways to cope with emotional changes and support those affected. Seeking support, practicing self-care, using non-verbal communication, focusing on the present, and remaining calm and patient can all make a significant difference in the emotional well-being of individuals with Alzheimer’s disease and their caregivers.