Personalized medicine is emerging as the future of Alzheimer’s drug development, offering new hope for patients and their families. This approach tailors treatments to individual patients based on their unique genetic makeup, lifestyle, and environmental factors.
Why is personalized medicine so promising for Alzheimer’s research? The answer lies in the complexity of the disease itself. Alzheimer’s affects each person differently, and what works for one patient may not work for another. By using personalized medicine, researchers can develop treatments that target specific aspects of the disease in each individual.
One exciting area of personalized medicine for Alzheimer’s is the use of genetic testing. Scientists have identified several genes associated with an increased risk of developing Alzheimer’s. By analyzing a patient’s genetic profile, doctors can better predict their risk and potentially intervene earlier with preventive measures or targeted therapies.
Another promising approach is the use of biomarkers. These are measurable indicators in the body that can signal the presence or progression of Alzheimer’s. For example, researchers are developing blood tests that can detect specific proteins associated with the disease. These tests could allow for earlier diagnosis and more personalized treatment plans.
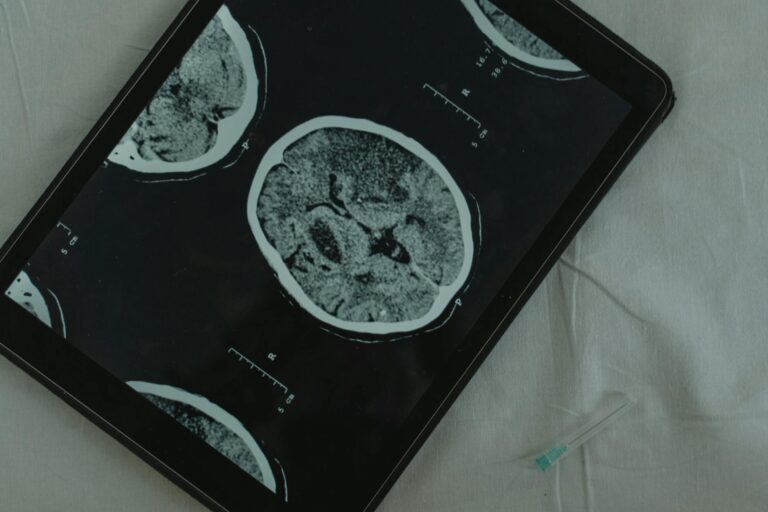
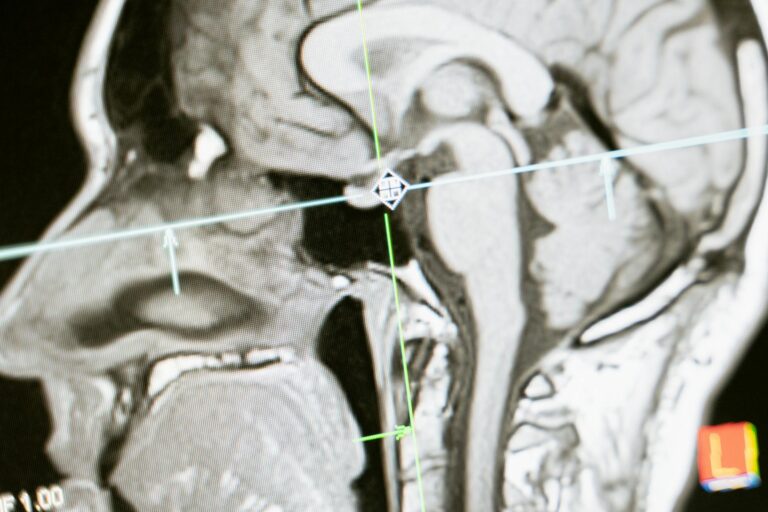
Advances in brain imaging techniques are also contributing to personalized medicine in Alzheimer’s research. High-resolution scans can now reveal detailed information about brain structure and function, helping doctors track the disease’s progression and tailor treatments accordingly.
The development of drugs that target specific molecular pathways involved in Alzheimer’s is another key aspect of personalized medicine. For instance, some new drugs aim to reduce the buildup of harmful proteins in the brain, while others focus on improving brain cell function. By matching these targeted therapies to patients based on their individual disease characteristics, researchers hope to improve treatment outcomes.
Clinical trials are adapting to the personalized medicine approach as well. Instead of testing drugs on large, diverse groups of patients, some trials now focus on smaller groups with specific genetic profiles or biomarker patterns. This approach can lead to more efficient drug development and potentially faster approval of new treatments.
Personalized medicine also extends to lifestyle interventions. Research has shown that factors like diet, exercise, and cognitive stimulation can affect Alzheimer’s risk and progression. By creating personalized prevention and management plans based on an individual’s unique risk factors and lifestyle, doctors can help patients take a more active role in their brain health.
While personalized medicine holds great promise, it also faces challenges. Developing individualized treatments can be more complex and costly than traditional approaches. There are also ethical considerations around genetic testing and data privacy that need to be addressed.
Despite these challenges, many experts believe that personalized medicine represents the best path forward in Alzheimer’s research. By tailoring treatments to each patient’s unique biology and circumstances, we may finally be able to make significant progress against this devastating disease.
As research continues to advance, we can expect to see more personalized approaches to Alzheimer’s prevention, diagnosis, and treatment. This shift towards individualized care offers new hope for millions of people affected by Alzheimer’s worldwide, potentially leading to more effective treatments and, ultimately, a cure.